Patients from poorer counties get worse hospital care, report finds
A report published last year from 3M’s Clinical and Economic Research division shows how Medicare patients living in lower-income and lower-education areas experience more preventable harm from hospital care, even after adjusting for patient risk.
The report also uses Lown Hospitals Index data, finding that hospitals with higher scores on LIHI Equity metrics also perform worse on certain preventable outcomes and patient safety metrics.
This study evaluated the impact of patient’s socioeconomic status (defined by their county’s income and education levels) on the performance of health care delivery around:
- Volume of hospitals admissions and emergency department visits (this shows how crowded the hospital might be)
- Readmissions and return emergency department visits (measures of post-acute care quality, measured as the difference between actual rates and expected performance, with risk adjustment)
- Inpatient complications and surgical mortality (measures of of inpatient care quality, measured as the difference between actual rates and expected performance, with risk adjustment)
The report found that Medicare beneficiaries in counties with low socioeconomic status (SES) had worse outcomes for many of these metrics compared to those in high-SES counties: There were more admissions and emergency department visits, more readmission and returns to the ED, more inpatient complications, and higher surgical mortality (see table below).
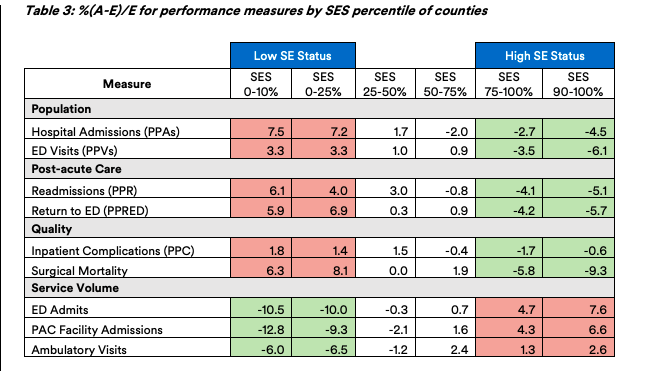
Low SES counties also had a higher proportion of dual-eligible Medicare-Medicaid patients (28% v 12%) and people of color (28% vs 15%) compared to high SES counties.
“These negative events indicate that the health care delivery system is not functioning as intended thereby creating heath care equity concerns,” the authors wrote.
The report also shows a correlation between socioeconomic status and performance on the Lown Hospitals Index. Hospitals with higher equity scores on the Lown Index were more likely to have a high proportion of patients in low-socioeconomic status counties. These high-equity hospitals were disproportionately on the low end of 3Ms quality of care measures, such as preventable admissions, readmissions, and surgical mortality (see table below).
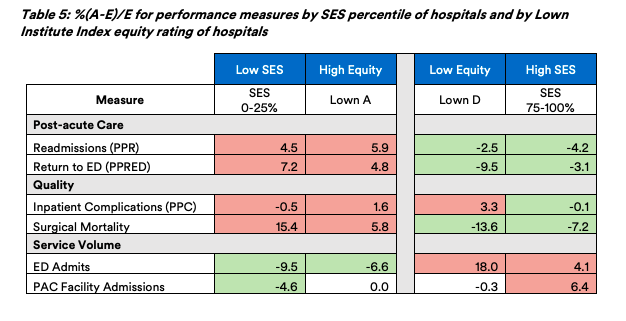
These patterns confirm a negative correlation we’ve previously seen on the Lown Index between equity and outcomes. This may be because risk adjustment does not account for certain unmeasurable socioeconomic factors, because safety net hospitals often operate with lower margins and fewer resources, or a combination of these factors.
However, the 3M report finds that inpatient complications were worse at hospitals with poor equity scores. This may be due to higher clinical complexity among patients going to large academic medical centers (many of which have low equity scores). Or it could mean that hospitals with low equity also lack processes to prevent inpatient complications.
Read the full report from 3M clinical and economic research here!
