For decades, cardiologists thought they knew why people with heart disease have angina, or chest pain: because of the plaque blocking their arteries. But a new study in The Lancet this week has rocked the world of cardiology by questioning whether stents are more effective than a placebo in relieving angina, and suggesting that blocked arteries aren’t the whole story.
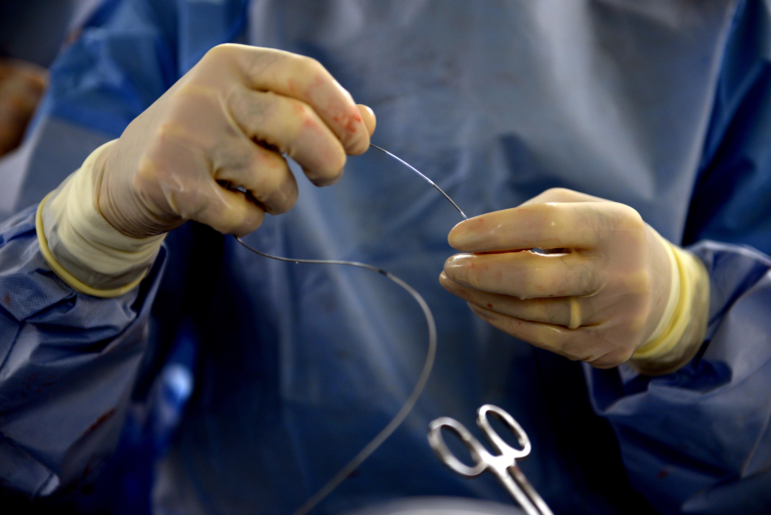
The ORBITA study was a double-blind, randomized controlled trial in which 200 patients with blockages in single vessels were given either a drug-eluting stent or a “sham” procedure. (A sham procedure is the surgical equivalent of giving a patient a placebo drug.) All patients received medication therapy for six weeks prior to the operation, and neither the patients nor the researchers who analyzed the results knew whether they had a been given a stent or placebo. When they measured patients’ pain and exercise time on a treadmill six weeks after the procedure, they found no difference between patients who really had their arteries opened and those who had the sham surgery.
Stents have been in widespread use for more than three decades for patients with heart disease, and several trials appeared to indicate that they were effective in reducing chest pain. But until now, that assumption has never been put to a real test in a placebo-controlled trial.
“This is mind-blowing,” said cardiologist and Lown Institute president Dr. Vikas Saini, “For cardiologists, this is like saying that penicillin doesn’t work for infections.” “Our capacity for serious skepticism was drowned out by the stampede to do more things.”
How could a mistaken concept be accepted for so many years without evidence? “Our capacity for serious skepticism was drowned out by the stampede to do more things,” said Saini, “And of course, there is a huge financial incentive to put in more stents.”
The implications of the ORBITA results can’t be understated, said Saini. “Think about how much money we spent on unnecessary stents over the decades and how many patients have been harmed from the complications!” he said. While the complication rate for angioplasty and stenting is relatively low, the number of patients who have undergone the procedure is tens of millions. The study also suggests that the placebo effect may be even more powerful than we’ve assumed.
In a Lancet editorial, cardiologists David Brown, professor of medicine at Washington University of St. Louis and co-chair of the Right Care Alliance cardiology council, and Rita Redberg, editor of JAMA Internal Medicine, call the ORBITA study “the last nail in the coffin” of controversy over stenting, especially for patients with stable coronary disease. When previous randomized trials showed that giving patients stents who are not in the throes of a heart attack, or at immediate risk for one, does not reduce their future risk of heart attack or death, the amount of stenting declined somewhat. But cardiologists have continued to use stents to relieve pain. Now, write Brown and Redberg, any stenting for patients with stable coronary disease is suspect.
The ORBITA study also calls into question the way in which the US Food and Drug Administration approves devices and their rapid adoption in the absence of valid evidence for efficacy and safety. While some physicians, including Redberg, Saini, and others have been calling for more sham trials for implantable medical devices, there has been considerable resistance from surgeons and device makers.
“There are risks to sham surgeries, but this study proves that they are absolutely necessary for evaluation,” said Saini.
Not all cardiologists agree with Brown and Redberg’s interpretation. Some note that the ORBITA trial only included patients with single vessel blockages, who were not experiencing severe symptoms of angina, and contend that patients with worse symptoms may benefit from stents.
That’s one reason why the need to replicate the study is critically important. “The ORBITA researchers have done a great service by giving us freedom to replicate,” said Saini. “Now it’s urgent that the government funds a large study to confirm these results. The stakes are too high to ignore.”