As many clinicians know, the problem with providing an unnecessary test or procedure is not simply the cost of that one service. When clinicians perform a diagnostic test or screening test “just to be safe,” it often leads to follow-up tests and procedures which are not only costly, but increases patient stress and the risk of harm from complications. For example, for every 10,000 women in their 40s who have annual mammograms, over ten years, 6,130 of those women will have a false positive test and 700 of those women will receive an unnecessary biopsy. None of these “cascade” events would have happened without the initial screening.
In a recent study in JAMA Internal Medicine, Dr. Ishani Ganguli at the Harvard Medical School and colleagues examines the downstream effects of a commonly overused procedure — electrocardiogram, or “EKG” (a test to detect heart problems), conducted before cataract surgery.
Cataract surgery is a low-risk, elective surgery. There is no evidence that routine cardiac before this surgery improves outcomes or lowers the risk of adverse events among Medicare beneficiaries, which is why guidelines do not recommend EKG before cataract surgery. However, it is still very commonly performed, costing Medicare an estimated $3.3 million each year.
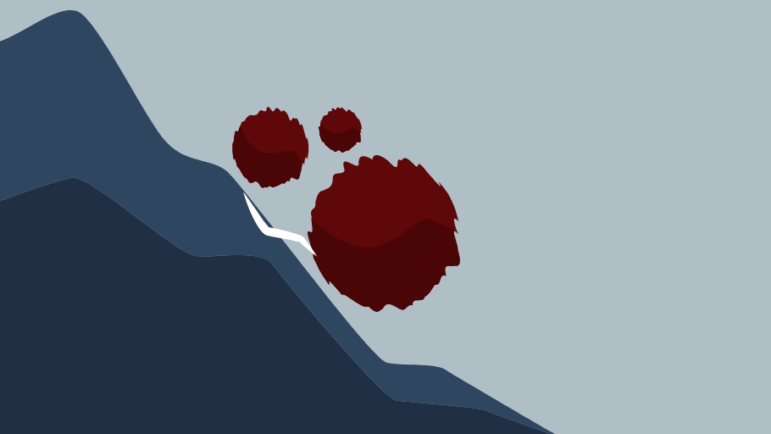
But that’s just the tip of the iceberg. Preoperative tests can lead to more follow-up tests, treatments, visits, hospitalizations, and new diagnoses. Ganguli et al calculated the prevalence and costs of these cascade events by analyzing Medicare claims data from one year, and comparing two groups of patients 90 days after routine cataract surgery — those who received preoperative EKG and those who didn’t.
They found that 16% of Medicare patients who received a preoperative EKG before cataract surgery experienced a cascade event within 90 days, such as another cardiac test, a cardiac specialist visit, and cardiac treatment. Of the patients who experienced at least one cascade event, more than half experienced more than one event, and a quarter of these patients had four or more!
Overall, “there were 5 to 11 cascade events per 100 beneficiaries, costing up to $565 per beneficiary or $35 million nationally in addition to $3.3 million for the initial electrocardiograms,” the authors write. The cost of unnecessary and harmful cascade procedures were ten times that of the cost for the initial low-value procedure!
This study has implications for measuring waste from low-value care. In a 2014 study, Harvard health economist Dr. Aaron Schwartz and colleagues found that just 31 common low-value care services cost Medicare $7 billion each year. However, they were not able to take into account downstream costs. A quick calculation of the cost from low-value tests and screenings in 2013 comes to about $3.3 billion (the rest of the $7 billion is from low-value surgeries and other procedures). Assuming that these tests and screenings have similar downstream costs as documented by Ganguli et al, that means that Medicare spends about $36.3 billion for just 23 low-value tests and the cascade of subsequent events. At nearly 5% of total Medicare spending, that’s nothing to sneeze at.